Understanding Acne Conglobata: Causes, Symptoms, X Treatments and More
Acne conglobata is a rare and severe type of acne that can sometimes develop from worsening pustular acne. It involves painful nodules and cysts that may merge, which can increase the likelihood of scarring. Management is important, as this condition can affect both skin health and emotional well-being. Because of its visible effects, it may also influence a person’s self-confidence.
In this article, we’ll explore the possible causes, common symptoms, and treatment options for acne conglobata. We’ll also look at long-term management strategies that may support skin health and overall well-being.
What is Acne Conglobata?
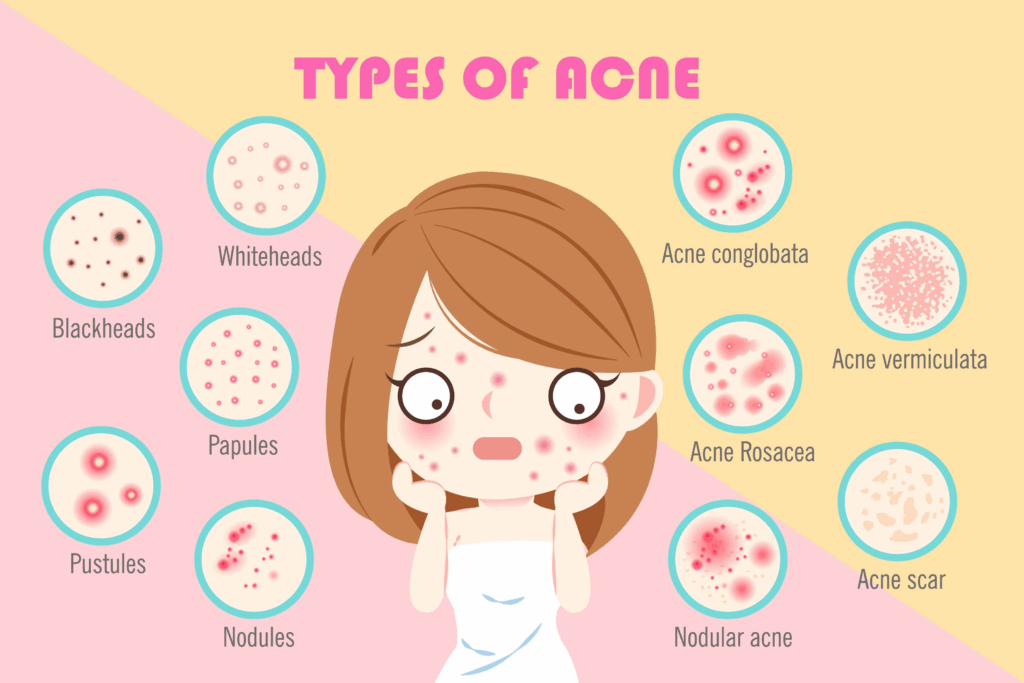
Acne conglobata is classified as a severe type of nodulocystic acne, with distinct features that set it apart from more common forms of acne. It is characterised by interconnected inflammatory nodules and cysts, which may cause discomfort and increase the risk of scarring. In this condition, the lesions can sometimes merge beneath the skin, creating more extensive areas of inflammation.
- Interconnected Nodules & Cysts: Unlike isolated pimples, acne conglobata may involve large, painful lumps that connect beneath the skin.
- Inflammation: Severe redness and swelling may occur, reflecting significant inflammation.
- Scarring Potential: Because of its severity, acne conglobata carries a higher risk of scarring, so timely medical assessment is advised.
Epidemiology and Prevalence
Typically, acne conglobata affects young men aged 18-30, though it can also occur in women. Hormonal changes during these years may contribute to its development. Genetic predisposition can also play a role, with some families showing a higher incidence of severe acne.
- Age Group: Predominantly affects individuals in their late teens to early thirties.
- Gender: More prevalent in males, possibly linked to testosterone levels.
- Genetic Links: Family history can increase risk, suggesting a genetic component.
Prevalence rates vary globally, but regions with higher humidity and pollution may see more cases, highlighting environmental influences alongside genetic factors.
Causes of Acne Conglobata
The development of acne conglobata is complex, involving biological, genetic, and environmental factors. Hormonal imbalances, particularly higher levels of androgens, are recognised contributors, as they can stimulate sebaceous glands and increase oil production.
Genetically, some individuals may be more prone to severe acne. In addition, bacteria such as Cutibacterium acnes (formerly Propionibacterium acnes) are involved in the inflammatory process. Environmental factors like high humidity, pollution, and stress may also contribute to flare-ups, reflecting the interplay between internal and external influences.
- Hormonal Imbalances: Higher levels of certain hormones may overstimulate oil glands and increase pore blockage.
- Genetic Predisposition: A family history of severe acne may raise the likelihood of developing acne conglobata.
- Bacterial Infections: Bacteria in blocked pores can trigger inflammation.
Risk Factors
While anyone can develop acne conglobata, some factors may increase the likelihood. A family history of severe acne is a recognised risk factor, suggesting a genetic predisposition. Certain medical conditions, such as hidradenitis suppurativa, may also raise the risk. Lifestyle elements, including diet, skincare routines, and stress management, can influence how acne develops, as can environmental factors like pollution and humidity.
- Family History: Genetic links can predispose individuals to severe forms of acne.
- Associated Conditions: Other skin conditions can exacerbate symptoms.
- Lifestyle and Environment: Diet, skincare, and environmental pollutants contribute to risk.
Symptoms
Acne conglobata presents with symptoms that set it apart from milder forms of acne. These include large, painful nodules and cysts that may connect beneath the skin’s surface. Inflammation is often marked, with redness and swelling. Pain and discomfort are common, and because of its severity, acne conglobata carries an increased risk of scarring.
- Nodules & Cysts: Large lumps that may merge, causing extensive inflammation.
- Pain and Inflammation: Severe discomfort with noticeable redness and swelling.
- Scarring: A high risk of permanent scars if not treated promptly.
Diagnosis
Diagnosis usually involves a clinical examination to distinguish acne conglobata from other forms of acne. Doctors typically assess the pattern and severity of nodules and cysts. In some cases, tests such as biopsies or bacterial cultures may be carried out to rule out other skin conditions.
- Clinical Examination: Doctors assess the pattern and severity of symptoms.
- Differentiation: Distinguishing from other acne types is key to treatment planning.
- Diagnostic Tools: Biopsies and cultures may be used to confirm the diagnosis.
Treatment Options
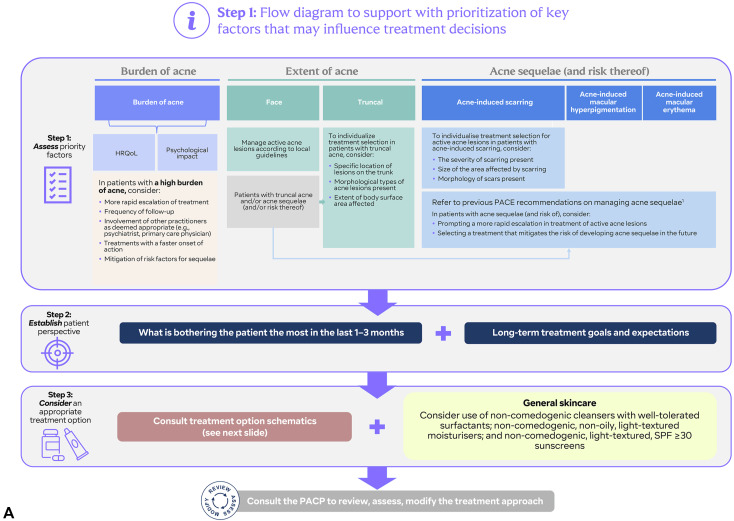
Management of acne conglobata often depends on the severity of the condition and individual factors. Different medical treatments may be considered as part of care.
Medical Treatments
Medical options may include both oral and topical medications. Oral antibiotics such as tetracycline are sometimes prescribed to manage bacterial involvement and inflammation. Isotretinoin may be prescribed for severe cases, as it acts on oil production and skin cell turnover. Topical agents like retinoids and benzoyl peroxide are used on the skin’s surface with the aim of keeping pores clear and managing inflammation.
- Antibiotics: Help control infection and reduce inflammation.
- Isotretinoin: A powerful drug for severe acne, addressing multiple causes.
- Topicals: Manage symptoms and prevent new outbreaks.
| Medication | Dosage | Potential Side Effects |
|---|---|---|
| Tetracycline | 1 mg/kg/d for 2–4 weeks | Nausea, vomiting, sensitivity to sunlight, dizziness |
| Doxycycline | 1 mg/kg/d for 2–4 weeks | Nausea, abdominal pain, photosensitivity |
| Isotretinoin | 0.5 to 1 mg/kg/day | Dry skin, chapped lips, mood changes, potential birth defects if pregnant |
| Benzoyl Peroxide | 2.5% to 10% topical, applied daily | Skin irritation, dry skin, peeling |
| Topical Retinoids | Once daily (variable potency) | Skin irritation, redness, photosensitivity |
| Clindamycin | 1% topical solution or gel, applied twice daily | Dry skin, irritation, and rarely diarrhoea |
This table provides an overview of common medications used in managing acne conglobata, along with general considerations such as possible side effects. Specific dosages are determined by a doctor and vary depending on individual needs.
Advanced and Surgical Treatments
For severe or resistant cases of acne conglobata, exploring advanced treatment options can provide additional strategies for relief. Advanced treatments include laser therapy and surgical interventions. Laser therapy targets bacteria and reduces inflammation, while surgical options may involve draining large cysts or removing damaged tissue. Corticosteroid injections can also reduce swelling and accelerate healing in stubborn acne nodules.
- Laser Therapy: Targets and reduces acne-causing bacteria.
- Surgical Interventions: Drains cysts and reduces severe inflammation.
- Corticosteroid Injections: Quickly reduce swelling and promote healing.
Complementary and Alternative Treatments
While medical treatments are commonly recommended for managing acne, complementary approaches may also support overall skin health. Home care practices, such as regular cleansing and hydration, may help maintain skin balance. Some people find that dietary adjustments, such as reducing dairy or high-glycaemic foods, are associated with fewer breakouts, although responses can vary.
In addition, lifestyle practices such as stress management or mindfulness may play a role in overall well-being, which can indirectly influence skin health. However, more research is needed to confirm the effectiveness of these approaches.
- Home Care: Consistent skincare routine with gentle products.
- Dietary Adjustments: Focus on balanced nutrition to support skin health.
- Emerging Treatments: Explore new therapies in conjunction with medical advice.
Complications and Long-term Effects
If left untreated or poorly managed, acne conglobata may result in long-term effects such as deep scarring or skin discolouration. In some cases, these changes may be addressed through medical or surgical procedures.
Additionally, chronic inflammation might increase the risk of systemic issues. Timely and effective treatment is crucial for minimising these risks and improving quality of life. Here’s a more detailed look at potential complications and long-term effects.
Potential Complications
Untreated or improperly managed acne conglobata can lead to various complications, notably scarring and secondary infections.
Scarring
One of the recognised risks of acne conglobata is scarring, which can sometimes be long-lasting. The inflammatory nature of this condition may damage the skin, resulting in pitted (atrophic) scars or raised (hypertrophic) scars. These changes can affect physical appearance and may also influence self-esteem or body image.
Secondary Infections
Inflamed nodules and cysts in acne conglobata may sometimes increase the risk of secondary infections. This may occasionally result in conditions such as cellulitis or abscesses, which could require additional treatment. Seeking early medical advice may help reduce the risk of such complications.
Psychological Impact
Severe acne conglobata may affect mental health, sometimes leading to social withdrawal, reduced self-confidence, or anxiety. In some individuals, these challenges may contribute to depression. Because of its visible effects, acne conglobata may also lead to feelings of isolation, highlighting the importance of psychological support alongside medical care.
Long-term Skin Management
Managing acne conglobata and supporting skin health requires ongoing care and preventive strategies. To help reduce flare-ups and support scar management, the following approaches may be considered:
- Consistent Skincare Routine: Establish a daily regimen that includes gentle cleansing, moisturising, and any targeted treatments as recommended by a doctor.
- Sun Protection: Use broad-spectrum sunscreen daily to help reduce the risk of worsening scarring or pigmentation changes.
- Regular Check-ups: Schedule regular appointments with a healthcare professional to monitor skin health, adjust treatment plans, and address concerns.
- Scar Treatment Options: Under professional guidance, treatments such as silicone gel sheets, chemical peels, or laser therapy may be considered for scar management.
- Healthy Lifestyle: A balanced diet, good hydration, stress management, and adequate sleep all support general health, which can play a role in skin condition.
- Avoid Picking or Squeezing: Refrain from manipulating acne lesions to lower the risk of further inflammation and scarring.
Preventing Acne Conglobata
Prevention and early intervention may help in managing acne conglobata. Adopting proactive measures may reduce the frequency of flare-ups and help lower the risk of long-term effects such as scarring or emotional distress.
Early Intervention Strategies
Early diagnosis and treatment may help slow the progression of acne conglobata and reduce the risk of complications, including scarring or infections. Recognising symptoms early and seeking professional advice may also support better long-term management. Key strategies include:
- Prompt Consultation: Seek medical advice at the first sign of severe acne lesions to allow for timely evaluation and recommendations.
- Regular Monitoring: Keep track of new or worsening symptoms to identify changes in the condition that may require adjusted treatment plans.
- Tailored Treatment Plans: Work with your doctor to develop personalised treatment approaches to target specific symptoms and skin types.
- Education on Skin Care: Understand the importance of using non-comedogenic skincare products and maintaining a consistent skincare routine.
- Awareness of Triggers: Identify and minimise potential triggers, such as stress, hormonal fluctuations, and dietary factors that may exacerbate breakouts.
- Support Systems: Engage with support groups or mental health professionals to address the emotional impact of acne and foster a supportive environment for recovery.
- Lifestyle Modifications: Adopt healthy habits, such as a balanced diet and regular exercise, to enhance overall skin health and resilience.
Lifestyle Modifications
Making conscious lifestyle adjustments can play a significant role in preventing the onset or worsening of acne conglobata. Here are some practical tips focusing on dietary changes, stress management, and effective skincare practices:
Dietary Adjustments
- Balanced Diet: Focus on a nutrient-rich diet with plenty of fruits, vegetables, whole grains, and lean proteins. Antioxidant-rich foods like berries and leafy greens can help combat inflammation.
- Limit Sugary and Processed Foods: Reduce intake of high-glycemic index foods, which can spike insulin levels and potentially trigger acne flare-ups.
- Stay Hydrated: Drink plenty of water throughout the day to maintain skin hydration and promote overall health.
- Consider Probiotics: Incorporate probiotic-rich foods, such as yoghurt and fermented foods, which may support gut health and, in turn, skin health.
Stress Management
- Mindfulness Practices: Engage in mindfulness techniques, such as meditation or deep-breathing exercises, to reduce stress and enhance emotional well-being.
- Regular Exercise: Incorporate physical activity into your routine, as exercise can alleviate stress and improve blood circulation, benefiting skin health.
- Adequate Sleep: Prioritise quality sleep by establishing a regular sleep schedule, as restorative sleep is essential for skin repair and overall health.
Skincare Practices
- Gentle Cleansing: Use a mild, non-comedogenic cleanser to remove impurities without irritating the skin. Avoid scrubbing, which can increase inflammation.
- Moisturise Regularly: Apply a suitable, oil-free moisturiser daily to maintain skin hydration while preventing excess oil production.
- Topical Treatments: As your doctor guides, consider incorporating topical treatments containing retinoids or salicylic acid to help manage existing lesions and prevent new breakouts.
- Avoid Irritants: Steering clear of harsh skincare products or physical irritants, such as exfoliating scrubs or rough fabrics, can prevent skin aggravation.
Psychological Impact of Acne Conglobata
Addressing the psychological implications of acne conglobata is an important aspect of overall care and well-being.
Emotional Distress
Acne conglobata can cause significant emotional distress, impacting mental health and quality of life. The visible nature of this condition can lead to self-consciousness or anxiety in social situations. Some individuals worry about their appearance, which may be linked to feelings of low mood or reduced self-esteem
Societal pressures and unrealistic beauty standards may further affect how people experience the condition. For this reason, psychological support such as therapy or support groups can provide coping strategies and a safe space to express feelings. Such support may encourage resilience and a more balanced self-image, complementing physical treatment.
Social Isolation
The social impact of acne conglobata extends beyond physical symptoms. Feelings of embarrassment or self-consciousness may sometimes lead individuals to withdraw from social activities. This can affect relationships, as loved ones may not always understand the emotional difficulties linked to the condition. Open communication and support from friends and family can play an important role in creating understanding and compassion.
Body Image Issues
Acne conglobata may affect body image, leading to negative self-perception or difficulty accepting one’s appearance. Visible lesions and scars can serve as reminders of the condition, sometimes resulting in harsh self-criticism or comparisons to societal ideals.
Supportive strategies may help address these challenges. Practising self-compassion, using positive affirmations, and engaging in body-positive activities such as support groups can provide encouragement. Professional support, including therapy or counselling, may also offer coping mechanisms for building a healthier self-image. Over time, these approaches may support resilience and foster a more positive relationship with one’s body.
When to See a Doctor

It’s important to consult a doctor if you suspect you have acne conglobata or if your acne symptoms worsen. Timely intervention can prevent scarring and manage symptoms more effectively.
- Consultation Triggers: Increased severity, pain, or scarring.
- Importance of Early Intervention: Prevents further complications.
- Professional Guidance: Tailored treatment plans based on individual needs.
For more information or to schedule a consultation, visit Lux Medical Aesthetic Clinic. Together, we can work towards achieving healthier, clearer skin. Our personalised care can provide comprehensive management tailored to your unique needs.
Conclusion
Going through the complexities of acne conglobata requires a complex approach, encompassing medical treatment, psychological support, and lifestyle modifications. Early diagnosis and comprehensive care are paramount in managing symptoms and preventing complications.
Remember, you’re not alone—help is available, and seeking professional guidance can make a significant difference in your skincare journey.