Back acne, or “bacne,” is a common skin condition where oil, dead skin cells, and bacteria clog hair follicles on the back, leading to inflammation and breakouts. The back’s thicker skin and harder-to-reach areas may present unique challenges in managing this condition compared to facial acne.
Understanding its causes, symptoms, and treatment options is essential for managing and preventing back acne.
What is Back Acne?
Back acne can manifest as blackheads, whiteheads, papules, pustules, nodules, and cysts. Due to the thicker skin on the back, deeper lesions and scarring may develop, which can sometimes present more persistent cases than facial acne. Commonly affected areas include the upper back, shoulders, and lower back.
Types of Back Acne
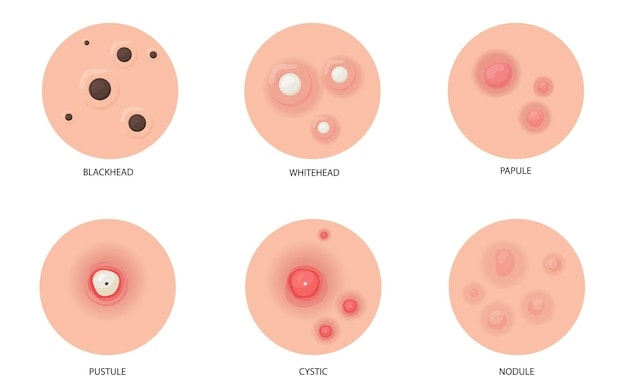
Back acne includes various types, such as:
- Comedones: Open (blackheads) and closed (whiteheads) comedones form when a pore is clogged with sebum and dead skin cells.
- Papules and Pustules: Inflamed lesions, often red and pus-filled bumps.
- Nodules and Cysts: Larger, deeper, and more painful lesions that are more likely to cause scarring if not treated properly.
Causes of Back Acne
Back acne develops due to a variety of factors, including hormonal changes, lifestyle habits, and external irritants.
Hormonal Changes
Fluctuations in hormones, particularly during puberty, menstruation, pregnancy, or stress, can increase oil production in sebaceous glands,which can clog pores and create an ideal environment for acne-causing bacteria to thrive. Hormonal back acne is often observed in teenagers and adults experiencing hormonal fluctuations or elevated stress levels. It is important to note that not all acne is linked to hormonal imbalances.
Sweat and Friction (Acne Mechanica)
Trapped sweat, tight clothing, and friction can exacerbate back acne in a condition known as acne mechanica. This type of acne is common in athletes or individuals who frequently wear backpacks or tight workout clothes. To minimise sweat-related acne, it’s advisable to wear loose, breathable fabrics and to shower immediately after sweating.
Bacterial Growth
The bacteria Cutibacterium acnes (formerly Propionibacterium acnes) thrive in clogged pores on sensitive skin, leading to inflammation and acne. Though this bacterium is part of the skin’s natural flora, rapid multiplication in clogged pores can lead to breakouts. Maintaining good hygiene and using appropriate antibacterial body washes can help reduce the bacterial load on the skin, potentially reducing acne breakouts.
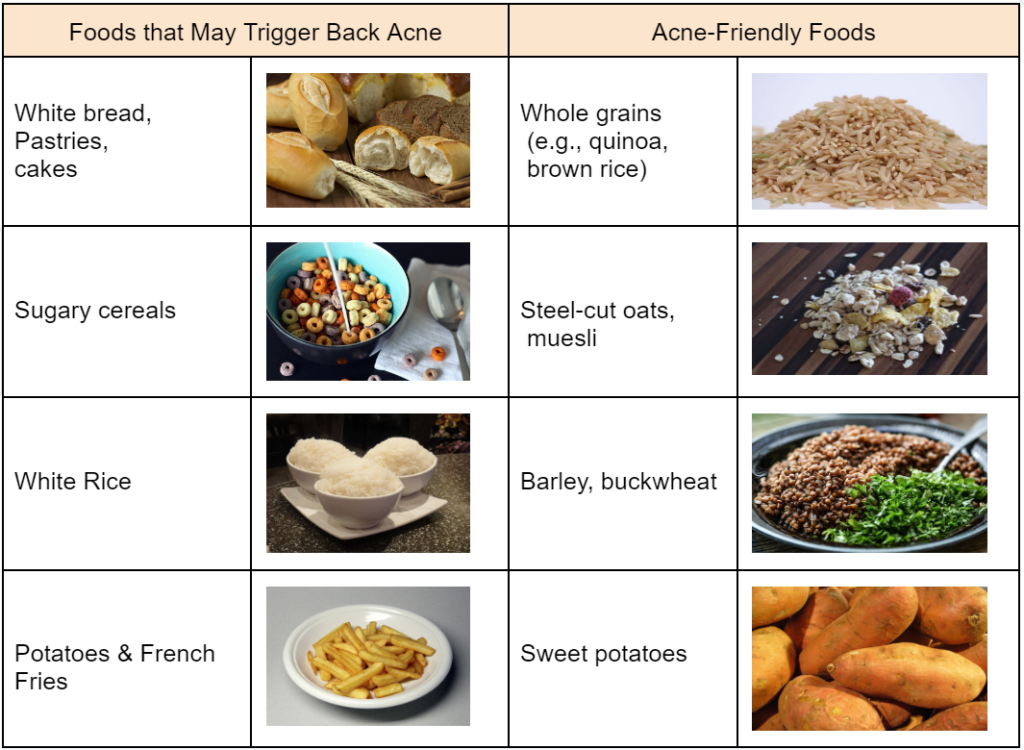
Dietary Impact
There is growing evidence that diet may influence acne. Studies suggest that high-glycemic foods, such as sugars and refined carbohydrates, may contribute to acne flare-ups by spiking insulin levels, which in turn can lead to increased sebum production. Some research also links dairy products to acne, particularly due to hormones present in milk. A diet focused on whole foods and low in processed sugars may help manage acne in certain individuals.
Poor Hygiene and Skincare
Inconsistent cleansing or using inappropriate skincare products may lead to back acne. Failing to clean the back regularly or applying products that clog pores can cause sweat, oil, and dead skin cells to build up, leading to blockages. Opting for non-comedogenic cleansers and exfoliating 1-2 times a week can also help remove dead skin cells.
Symptoms and Severity of Back Acne
Back acne can vary in severity from mild to severe. Symptoms commonly include redness, inflammation, and discomfort. The severity is often assessed based on the number and type of lesions present as well as the degree of skin inflammation. Mild cases may involve a few scattered pimples and minor irritation, while more severe cases can present with numerous, inflamed lesions such as cysts and nodules, leading to significant pain and potential scarring. The overall impact on daily life and skin appearance can help determine the appropriate level of treatment required.
Treatment Options for Back Acne
There are various back acne treatment options including topical medications readily available at drugstores, prescription treatments, and professional interventions if necessary.
Over-the-Counter Treatments
OTC products like salicylic acid, benzoyl peroxide, and alpha hydroxy acids (AHAs) are commonly used to treat back acne. These ingredients help exfoliate the skin, unclog pores, reduce inflammation, and kill acne-causing bacteria.Body washes or sprays specifically formulated for acne-prone skin are recommended for daily use.
Prescription Medications
For more severe cases, prescription treatments such as topical retinoids, oral antibiotics, and hormonal therapies (like oral contraceptives) may be recommended. These treatments target inflammation, reduce bacteria, and help control oil production. In cases of severe cystic acne, isotretinoin, a powerful oral retinoid, may be prescribed under strict medical supervision.
Professional Treatments
Chemical peels, laser therapy, and light therapy are some of the professional treatments available for back acne. These treatments aim to reduce acne lesions, control oil production, and address acne scarring. Consulting a dermatologist is essential to determine the most suitable professional treatment based on individual needs.
Home Remedies and DIY Approaches
Some people use natural remedies, such as tea tree oil, aloe vera, and honey, for mild cases of back acne, although their effectiveness can vary. While some individuals may find relief using these natural treatments, they should be used cautiously, as they might not be effective for everyone and could potentially irritate the skin.
Skincare Routine

A consistent skincare routine is important in managing and preventing back acne. This includes using acne-friendly skincare products such as a gentle cleanser, exfoliating regularly, and moisturising the skin to maintain its barrier function without clogging pores.
Preventing Back Acne
Preventing back acne requires a proactive approach focusing on proper hygiene, skincare, clothing choices, diet, and lifestyle changes. Understanding the triggers can reduce the occurrence and severity of back acne.
Maintaining Proper Hygiene
Regular cleansing is crucial for preventing back acne. Sweat and bacteria can accumulate on the skin’s surface leading to breakouts. Here are some hygiene tips that may help reduce the occurrence of back acne:
- Shower promptly after sweating or any activity that causes perspiration.
- Use gentle, non-comedogenic cleansers to remove dirt, oil, and sweat to help maintain clear skin.
- Exfoliate the back 1-2 times a week to remove dead skin cells that can clog pores.
- Avoid harsh scrubbing as it can irritate the skin and worsen acne.
Choosing the Right Clothing
Tight-fitting clothes, especially those made from synthetic materials, can trap sweat and bacteria against the skin, exacerbating acne. Change out of sweaty clothes immediately to prevent bacteria from sitting on the skin.
Wearing loose, breathable fabrics like cotton is also better suited for those prone to back acne, as they allow the skin to breathe and help reduce moisture buildup. Regularly wash clothes, especially those worn during exercise, to remove sweat, bacteria, and oils.
Diet and Lifestyle Factors
Diet and lifestyle factors significantly impact the severity and frequency of back acne. Consuming high-sugar foods and refined carbohydrates can trigger insulin spikes, leading to increased production of sebum and acne outbreaks.
- Staying hydrated, eating a balanced diet rich in fruits, vegetables, and whole grains, and managing stress through activities like meditation or exercise can reduce the risk of acne flare-ups.
- Manage stress by engaging in activities such as yoga, meditation, or exercise to prevent hormone-induced acne flare-ups.
- Get adequate sleep to help regulate hormonal levels, potentially reducing acne breakouts.
Avoiding Common Triggers
Certain products and habits can worsen back acne. Listed below are common triggers to avoid:
- Refrain from using heavy or greasy lotions and sunscreens.
- Avoid letting shampoos and conditioners run down your back during rinsing.
- Do not pick or pop acne lesions to avoid further irritation, infection, and potential scarring.
- Limit sun exposure to prevent post-inflammatory hyperpigmentation and long-term skin damage.
Regular Monitoring and Maintenance
Regularly monitoring the skin on your back and maintaining good skincare practices is essential to prevent back acne. Be mindful of any changes in the skin, such as new breakouts or irritation, which might indicate a reaction to a new product or environmental factor.
Dos and Don’ts for Maintaining Clear Skin:
- Do cleanse daily: Use a gentle cleanser suited for acne-prone skin.
- Don’t skip moisturising: Even oily skin needs hydration; choose oil-free, non-comedogenic moisturisers.
- Do use acne treatments as needed: Spot treatments with salicylic acid or benzoyl peroxide can help target specific breakouts.
- Don’t ignore persistent acne: If acne does not improve with over-the-counter products or becomes painful, consult a dermatologist for professional advice.
Myths and Misconceptions About Back Acne
Bacne is often misunderstood, with several myths and misconceptions surrounding its causes and treatment. Understanding the difference between back acne and other forms of body acne and debunking common myths can help individuals manage this condition more effectively.
Back Acne vs. Body Acne
Myth: Back acne is the same as other types of body acne.
Fact: Body acne can show up on the chest, shoulders, and buttocks, but bacne is persistent due to the skin’s thickness and the higher density of sebaceous glands on the back. This leads to deeper cysts and nodules, which are more difficult to treat and more likely to cause scarring.
Natural Remedies and Back Acne
Myth: Natural remedies, such as tea tree oil or apple cider vinegar, are effective treatments for back acne.
Fact: While some natural products have antibacterial or anti-inflammatory properties, their effectiveness varies among individuals and should be used cautiously. For example, tea tree oil can be beneficial for mild acne due to its antimicrobial qualities, but incorrect use may cause skin irritation. Similarly, apple cider vinegar is promoted as an acne remedy because of its acidic nature, but undiluted application can disrupt the skin’s pH balance, potentially causing irritation or burns.
Impact of Back Acne on Quality of Life
Back acne can significantly impact both physical comfort and psychological well-being.
Physical Discomfort and Scarring
Back acne, especially when involving nodules or cysts, can cause considerable physical discomfort, including pain and itching. These deeper lesions are more likely to result in acne scarring, which can be:
- Hypertrophic (raised scars)
- Keloid (larger, raised scars that extend beyond the initial wound)
- Atrophic (sunken scars)
Managing active acne and promptly treating scars are crucial to minimising long-term skin damage and scarring. Tips for preventing and treating acne scars on the back include avoiding picking or squeezing lesions, using sunscreen to protect healing skin, and considering professional treatments like chemical peels, laser therapy, and microneedling to reduce the appearance of scars.
Psychological and Social Effects
Many individuals experience reduced self-esteem and confidence due to visible acne lesions, particularly in social gatherings. This can lead to social withdrawal and emotional distress, especially among teenagers and young adults. Addressing these psychological impacts is as important as treating the physical symptoms.
How to Address the Emotional Impact of Back Acne:
- Develop a consistent skincare routine for overall skin health and improve self-confidence.
- Connect with others who have similar experiences to reduce feelings of isolation.
- Consult a dermatologist or a mental health professional for expert guidance and reassurance.
When to See a Dermatologist

While mild cases of back acne can often be managed with over-the-counter treatments and lifestyle changes, more severe cases may require professional intervention. Here are some indications that back acne might need medical attention:
- Persistent, severe acne that does not respond to home treatments.
- Development of painful, cystic acne that causes significant discomfort.
- Noticeable scarring or changes in skin texture.
- Emotional distress related to the appearance of acne.
For more information on professional treatments and personalised advice, you may consult a dermatologist or visit Lux Medical Aesthetic Clinic services page.
Conclusion
Back acne can be a persistent and challenging condition, but understanding the causes, symptoms, treatments are crucial steps toward effective acne management. By taking a comprehensive approach that includes proper skincare, lifestyle adjustments, and seeking medical treatments when necessary, individuals can better manage their skin health and improve their quality of life.