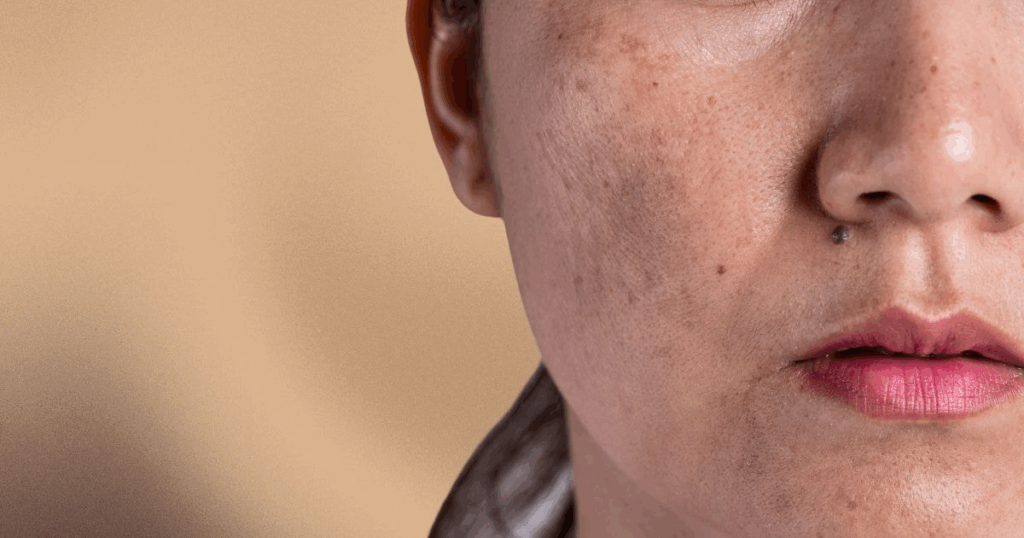
Melasma is a common skin condition characterised by brown or grey-brown patches, often on the face. It primarily affects women and can be influenced by hormones, sun exposure and genetics.
This guide covers what causes melasma, its symptoms and treatment options to help you manage and prevent it.
What is Melasma?
Melasma is a type of hyperpigmentation that causes dark patches on the face, especially the cheeks, forehead, nose and upper lip. It is triggered by excessive melanin production and tends to worsen with frequent sun exposure. While not harmful, melasma can cause significant skin discolouration, which may impact appearance and self-esteem.
How Common is Melasma?
Studies show that melasma affects 15 to 50% of pregnant women and up to 30% of the general population in certain regions. It’s most common in people with darker skin tones, such as those of Asian, Hispanic or African descent. However, anyone can develop melasma, regardless of their ethnicity.
Causes of Melasma
Melasma results from a combination of internal and external factors, with some key triggers including:
- Hormonal changes. Fluctuations in estrogen and progesterone levels are commonly known as the ‘mask of pregnancy’ due to their frequent occurrence in pregnant women. Hormonal changes increase melanin production in certain areas of the skin, leading to the formation of dark patches. According to a report, between 1.5% and 33% of the population may get melasma and women are more prone to developing melasma, particularly during their third trimester of pregnancy.
- Sun exposure. Ultraviolet (UV) light is one of the main external factors contributing to melasma. UV rays stimulate the production of melanin pigments, which leads to the darkening of existing melasma patches and the development of new ones. Visible light and infrared radiation can also worsen melasma, making sun protection crucial in managing the condition.
- Genetics. Genetics also plays a role in melasma development. If there is a family history of melasma, the chances of developing it increase significantly.
- Medications. Certain medications like antiseizure medications, phototoxic drugs and some oral contraceptives may increase or worsen melasma. These drugs may cause the skin to become more sensitive to sunlight, thereby enhancing melanin production in affected areas. Some medications may also lead to skin reactions that result in post-inflammatory hyperpigmentation, mimicking or exacerbating melasma.
Types of Melasma
Melasma is categorised into three types based on how deeply the pigmentation affects the skin:
Epidermal Melasma
This type involves epidermal pigment, appearing as dark brown patches that affect the outermost layer of the skin. This type generally responds well to skin-lightening treatments, such as hydroquinone or azelaic acid.
Dermal Melasma
This penetrates deeper into the skin, producing blue-grey patches. Dermal melasma is more difficult to treat, as the dermal pigment lies in the deeper layers, making it resistant to many surface-level treatments. Patients may require more intensive therapies like laser treatments to target these pigments.
Mixed Melasma
This form of melasma features both epidermal and dermal pigmentation, resulting in patches that appear brown and grey. Due to its involvement of multiple skin layers, mixed melasma can be more difficult to treat effectively.
Distribution Patterns of Melasma
Melasma can be classified by the depth of pigmentation and its distribution on the face. Recognising these patterns helps diagnose melasma and tailor suitable treatment plans. The three main patterns are:
Centrofacial Pattern
This is the most common pattern, affecting the cheeks, nose, forehead, upper lip and chin. These areas are more exposed to sunlight, making them more susceptible to melasma. UV light and visible light are major triggers in these areas, stimulating melanin production and worsening melasma and other pigmentary disorders.
The centrofacial pattern often requires a more comprehensive treatment plan, as the larger surface area demands careful application of sun protection and topical treatments across various regions of the face.
Malar Pattern
The malar pattern affects the cheeks and nose, areas that are also highly prone to sun exposure. Due to its prominent position on the face, this pattern can be more noticeable and can worsen with prolonged UV exposure.
People with darker skin tones are more susceptible to malar melasma, and this pattern is frequently seen in individuals with Asian skin or other deeply pigmented skin types. This pattern is often managed with topical medications like azelaic acid and hydroquinone, combined with chemical peels for effective skin lightening.
Mandibular Pattern
The mandibular pattern is the least common form of melasma and occurs along the jawline. While less frequent, it can be challenging to treat due to the area’s skin thickness. The mandibular pattern is often accompanied by other melasma patterns, which complicates treatment. In many cases, this pattern may be linked to hormonal changes, particularly in pregnant women, and might require a combination of oral treatments, topical therapies and systemic treatments.
Treatment Options for Melasma
Although there is no permanent cure, several treatments can help manage melasma. A comprehensive treatment plan usually includes multiple approaches to minimise pigmentation.
Topical Treatments

Topical creams are a first-line treatment for melasma. Common options include:
- Hydroquinone. This commonly used skin-lightening agent works by blocking the enzyme tyrosinase, which is necessary for melanin production. It is available in concentrations ranging from 2% to 4%. However, prolonged use may lead to complications such as hydroquinone-induced exogenous ochronosis, a condition where bluish-black pigmentation develops. Due to these risks, it is usually used for short periods and under medical supervision.
- Kojic acid and azelaic acid. These ingredients are milder alternatives and are often used for long-term management. Kojic acid inhibits tyrosinase, while azelaic acid works by reducing the number of abnormal melanocytes. Both are used in lightening dark patches and are generally well-tolerated.
- Tretinoin and corticosteroids: Tretinoin (a vitamin A derivative) can increase skin cell turnover, which may help to shed pigmented cells faster. It can be combined with hydroquinone and corticosteroids to reduce inflammation and improve the overall effectiveness of the treatment.
Chemical Peels and Microdermabrasion
Chemical peels are suitable second-line treatment for patients who do not respond well to topical agents alone. This procedure involves the application of acids like glycolic acid or trichloroacetic acid (TCA) to exfoliate the outer layer of the skin, revealing newer, less pigmented skin underneath. Chemical peels also stimulate skin cell production to improve skin texture and even out tone.
There are three main types of chemical peels used for melasma:
- Superficial peels. These target the outermost layer of skin and are commonly used for epidermal melasma.
- Medium-depth peels. Used for more persistent pigmentation, these penetrate deeper into the skin.
- Deep peels. Though rare, these are reserved for the most severe cases, and they carry more risk of complications.
Multiple sessions are usually necessary for visible improvement, and combining peels with topical hydroquinone can prevent new pigment formation.
Laser Treatment
Laser therapies and light-based treatments can help reduce melanin pigments in the skin. These are typically considered for cases that do not respond to topical or chemical treatments. Common laser treatments include:
- Q-switched laser. This device delivers short bursts of energy that may help break down melanin pigments into smaller particles, which the body can gradually absorb.
- Pico Laser: Pico Laser uses ultra-short pulses of laser energy measured in picoseconds to target pigment in the skin. The rapid bursts of energy help fragment melanin into finer particles, which are then cleared by the body’s natural processes. It is commonly used to manage conditions like melasma, pigmentation, and uneven skin tone, while supporting skin rejuvenation with minimal downtime.
It is essential to approach laser treatments cautiously, as improper use may worsen melasma or lead to scarring.
Oral Medications
Oral treatments may be considered for more resistant cases of melasma. One of the most promising options is tranexamic acid, an oral medication that helps reduce melanin production by blocking the interaction between melanocytes and blood vessels. It is particularly useful in patients who do not respond to topical treatments or those with mixed melasma.
While tranexamic acid has shown good results in reducing pigmentation, it is typically reserved for short-term use due to potential side effects, such as gastrointestinal disturbances. A healthcare professional will monitor patients closely during treatment.
Prevention Strategies for Melasma
While treatment can help reduce the appearance of melasma, prevention is key to managing the condition long-term and minimising future flare-ups. Effective prevention strategies focus on reducing exposure to common triggers and maintaining proper skin care habits. Here are some tips:
Use Sun Protection
A key step in preventing melasma is sun protection. Ultraviolet (UV) radiation is a major trigger for melasma, as it stimulates melanin production and can worsen existing pigmentation. To protect your skin:
- Apply broad-spectrum sunscreen with an SPF of at least 30 daily, even on cloudy days. Sunscreens containing zinc oxide, titanium dioxide and iron oxides offer the best protection from UV and visible light.
- Reapply sunscreen every two hours, especially if you’re outdoors or swimming.
- Wear protective clothing, like wide-brimmed hats, long sleeves and sunglasses, to shield your skin from direct sunlight.
- Avoid peak sun hours from 10 AM to 4 PM.
Be Aware of Hormonal Triggers
Hormonal changes are a leading cause of melasma, particularly in pregnant women and those taking birth control pills or hormone replacement therapy. If you’re using oral contraceptives or other hormonal medications, discuss alternative options with your healthcare provider to potentially avoid triggering melasma. Pregnancy-related melasma often fades after delivery, but women should still take preventive measures during pregnancy to avoid worsening the condition.
Seek Early Treatment
Early intervention is essential when melasma appears. Seeking treatment at the first sign of skin discolouration can prevent the condition from worsening. Topical treatments can help manage melasma early on, especially when combined with proper sun protection.
Maintain Treatment
Even after achieving improvement, melasma can recur, particularly with continued exposure to sunlight or hormonal changes. It’s essential to maintain treatment with strict sun protection and ongoing maintenance therapy, such as the use of skin-lightening agents or topical medications. Consistent care can help prevent relapse.
Can melasma go away on its own?
In some cases, melasma may fade without treatment, especially if it was triggered by pregnancy or hormonal medications like birth control pills. However, melasma often requires long-term management and may persist or worsen without proper care.
Is melasma the same as hyperpigmentation?
While melasma is a specific form of hyperpigmentation, it is distinct in its causes and triggers. Melasma is often caused by hormonal fluctuations, sun exposure or genetics, whereas other types of hyperpigmentation, such as post-inflammatory hyperpigmentation, can result from skin injuries or allergic reactions.
Conclusion
Melasma is a chronic skin disorder that requires both preventive measures and effective treatments for management. Protecting your skin from sun exposure, being mindful of hormonal changes and seeking early treatment are critical strategies to control melasma. Ongoing care and sun protection can help prevent relapse and keep your skin looking healthy.
Struggling with melasma? Get in touch with Lux Medical Aesthetic Clinic, and regain your radiant complexion.