Acne is a common skin condition that many experience at some point, especially during adolescence. Its impact extends beyond physical appearance, often affecting self-esteem and overall well-being. This guide will cover acne, its causes, symptoms, types, and various treatment options. It aims to provide valuable information to those affected by acne, helping them better understand the condition and explore ways to manage and treat it.
What is Acne?
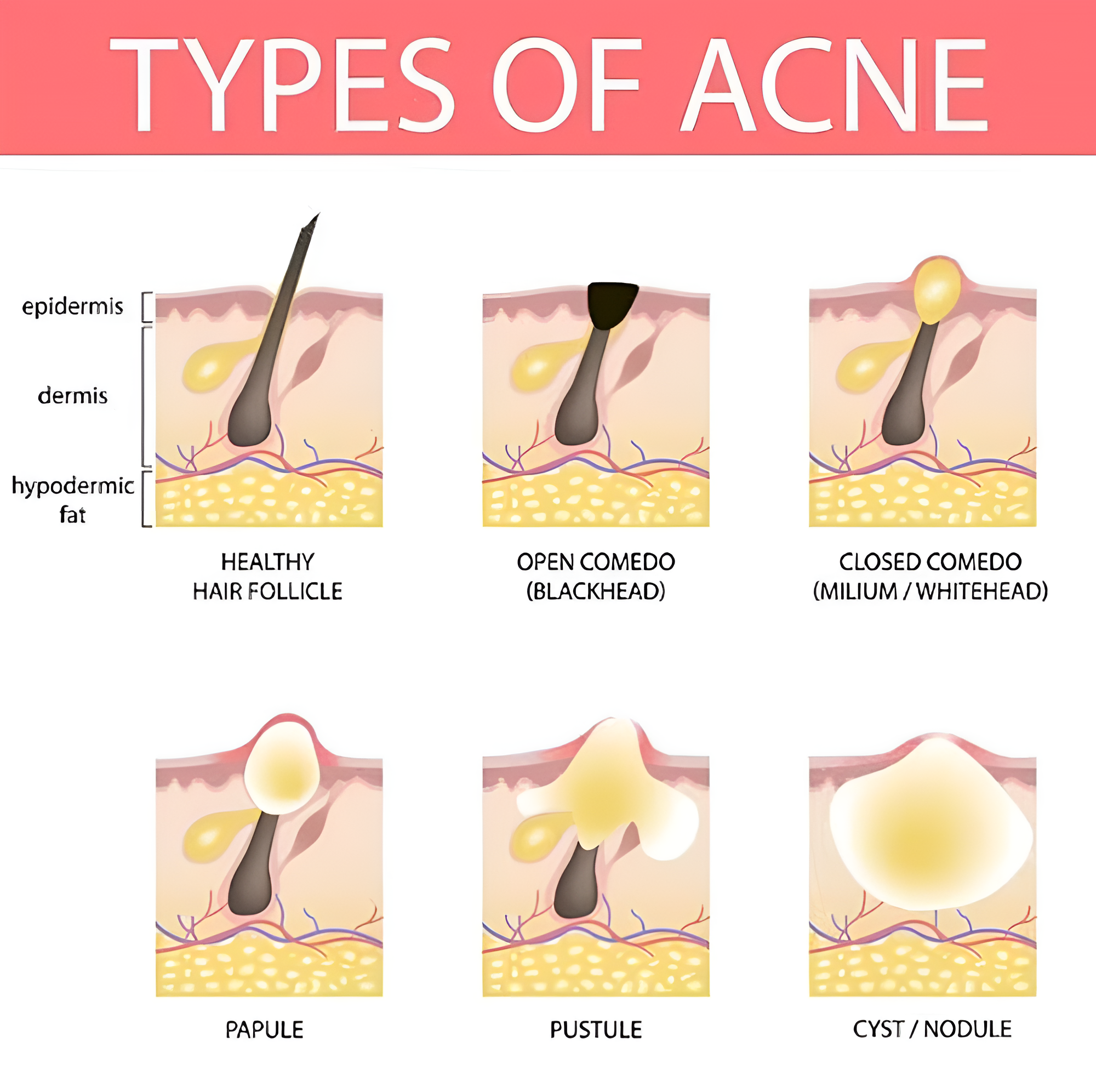
Acne is a skin condition when hair follicles become clogged with oil and dead skin cells. It is most prevalent among teenagers, though it can affect people of all ages. Acne appears in various forms, including whiteheads, blackheads, pimples, and cystic acne lesions.
According to a study in Singapore, 88% of teenagers report experiencing some form of hormonal acne themselves. This statistic highlights how common the condition is.
Impact on Self-Esteem
Acne can affect one’s self-esteem and mental health. Many individuals with acne report feeling self-conscious or anxious about their appearance, often avoiding social interactions and public events. This emotional toll can lead to feelings of isolation and depression, making it a critical factor to consider when discussing acne and its treatment.
Addressing acne’s physical and psychological aspects is essential for providing comprehensive care and support to those affected.
What are the Signs and Symptoms of Acne?
Acne symptoms vary, but they typically include several common indicators. These can range from mild to moderate severity and may appear differently depending on the individual. Some common signs of acne include:
- Whiteheads: These are closed plugged pores that appear as small, white bumps on the skin’s surface.
- Blackheads: These are open plugged pores that look dark on the surface due to the oxidation of trapped debris.
- Papules: These are small, red, tender bumps that form when hair follicles become inflamed or infected.
- Pustules: These are pimples with pus at their tips, often resulting from a pore infection.
- Nodules: These are large, solid, painful lumps located deep beneath the skin’s surface, often caused by severe inflammation.
- Cysts: These are painful, pus-filled lumps beneath the skin’s surface, usually resulting from severe infections and can lead to scarring.
What Causes Acne?
Several factors contribute to the development of acne, including:
Excess Oil Production (Sebum)
The sebaceous glands in the skin produce an oily substance called sebum. This natural oil helps to keep the skin moisturised and protected. However, when sebum is produced in excess, it can mix with dead skin cells and other debris, clogging pores and developing acne. This is particularly common in the T-zone, where many people experience forehead acne.
This can result in various forms of acne, such as black and whiteheads or more severe inflammatory lesions. Good skincare and hygiene can help manage sebum production and reduce the risk of clogged pores.
Clogged Pores with Dead Skin Cells
Dead skin cells can accumulate on the skin’s surface and mix with excess oil, leading to clogged pores. This buildup and skin irritation can result in various skin issues, including acne, blackheads, and dull complexion. Regular exfoliation and proper skincare routines are essential to remove these dead cells and maintain healthy, clear skin.
Bacterial Growth
Propionibacterium acnes (P. acnes) can grow in clogged pores and thrive in an oxygen-poor environment. This growth often leads to inflammation, causing the immune system to react and forming pimples and other acne-related symptoms. Understanding the role of P. acnes helps in developing acne treatments.

Inflammation
The inflammatory response in the skin can cause redness (skin discoloration), swelling, and pain, further exacerbating acne. This inflammation often occurs when pores become clogged with excess oil, dead skin cells, and bacteria, forming pimples, cysts, and other blemishes.
Over time, the persistent inflammation can damage the skin and contribute to scarring, making it essential to manage both the inflammation and the underlying causes of acne.
What are the Risk Factors for Acne?
Several risk factors can increase the likelihood of developing acne:
- Age: Teenagers and young adults are more prone to acne due to hormonal changes that occur during puberty. These hormonal shifts can lead to increased oil production and clogged pores, the primary causes of acne.
- Hormonal Changes: Puberty, menstruation, and pregnancy can trigger hormonal fluctuations that lead to acne. For example, elevated levels of androgens during puberty stimulate the sebaceous glands in the skin, resulting in more oil production and potential breakouts.
- Genetics: A family history of acne increases the likelihood of developing the condition. If your parents or close relatives had acne, you may be genetically predisposed to experiencing similar skin issues.
- Certain Medications: Drugs containing corticosteroids, androgens, or lithium can cause severe acne. These medications may alter hormone levels or affect the skin’s oil production, leading to breakouts.
- Diet: High glycemic foods might contribute to acne, though research is ongoing. Foods that cause a rapid spike in blood sugar levels can increase insulin levels, which may, in turn, boost oil production and inflammation in the skin.
Stress: Stress can worsen acne by increasing hormone levels that stimulate oil production. When you’re stressed, your body produces more cortisol and other stress-related hormones, which can lead to more oil production and clogged pores.
Types of Acne
Comedonal Acne
Comedonal acne primarily consists of blackheads and whiteheads. Blackheads, or open comedones, appear when pores are clogged with oil and dead skin cells. The pore’s surface remains open, and the accumulated substances oxidise, turning black.
Whiteheads, or closed comedones, form when the clogged pore closes up, creating a small bump under the skin. Both types of comedonal acne are non-inflammatory and generally less severe than other forms of acne.
Inflammatory Acne
Inflammatory acne includes papules, pustules, nodules, and cysts, typically characterised by redness, swelling, and pain:
- Papules: Small, red, tender bumps that occur when the walls surrounding the pores break down due to severe inflammation.
- Pustules: Pimples containing pus at their tips. They appear red at the base with a white or yellow head.
- Nodules: Large, solid, and often painful lumps beneath the skin’s surface. Nodules can be more challenging to treat because they form deeper within the skin.
- Cysts: Painful, pus-filled lumps akin to nodules, but cysts are filled with pus. They can cause significant scarring due to their severity and depth within the skin.
Each type of inflammatory acne varies in severity and requires different treatment approaches to manage effectively.
When to See a Professional
Consulting a medical or aesthetic practitioner is recommended in the following situations:
- Severe or cystic acne
- Persistent acne that doesn’t respond to over-the-counter treatments
- Acne that leads to scarring or dark spots
- Emotional distress due to acne
How Can You Manage Acne?
In addition to prescribed treatments, some self-care methods can help manage and prevent acne breakouts.
- Gentle Cleansing Routine: Wash your face twice daily with a gentle, non-comedogenic cleanser. Avoid over-washing, as this can strip the skin of its natural oils and increase oil production. Using lukewarm water instead of hot water can also help prevent further irritation and dryness.
- Non-comedogenic Skincare Products: Use products labelled as non-comedogenic, meaning they are less likely to clog pores. This includes moisturisers, sunscreens, and makeup. Look for products containing beneficial ingredients, such as hyaluronic acid for hydration or niacinamide for soothing inflammation.
- Avoiding Harsh Scrubs and Irritants: Avoid abrasive scrubs and ingredients that irritate the skin, such as alcohol-based products and fragrances. These can exacerbate acne and lead to further inflammation. Instead, opt for gentle exfoliants like salicylic acid or lactic acid, which can help to clear pores without irritating them.
- Reducing Stress: Incorporate stress-management techniques into your daily routine, such as yoga, meditation, or adequate sleep. Lowering stress levels can help balance hormone levels and reduce breakouts. Practising mindfulness or engaging in hobbies you enjoy can contribute to overall mental well-being, which may also reflect in your skin.

Maintaining a Healthy Diet: Opt for a balanced diet rich in fruits, vegetables, and lean proteins. Avoid high glycemic index foods and processed items, as they can spike insulin levels and potentially worsen acne. Additionally, consider incorporating probiotics, as emerging research suggests they positively impact skin health. Foods rich in omega-3 fatty acids, like salmon and walnuts, can also support skin health by reducing inflammation.
Conclusion
Acne is a common yet complex condition that affects many individuals, especially young adults. Understanding the causes, symptoms, risk factors, and treatment options is crucial in managing acne effectively. While over-the-counter treatments and lifestyle changes can help, seeking advice from a professional is beneficial.
If you’re struggling with acne, remember that you are not alone, and there are various ways to manage and treat the condition. Take the first step in managing your skin health by exploring available treatment options and consulting a professional for advice.